What Causes Irritable Bowel Syndrome is a common question for those experiencing chronic digestive problems. Understanding the factors behind IBS can help people manage symptoms and improve gut health. This article explores the causes, triggers, and strategies for finding relief.
Living with IBS can be challenging, ongoing discomfort, abdominal pain, unpredictable bathroom trips, and bloated gut pain can disrupt daily routines. Recognizing early signs of gastrointestinal disease allows timely care and strategies to reduce symptoms and improve quality of life.
What is Irritable Bowel Syndrome?
Irritable Bowel Syndrome (IBS) is a chronic disorder of the digestive tract, causing abdominal discomfort and changes in bowel habits, such as diarrhea, constipation, or both. Unlike structural diseases, IBS affects gut function rather than its physical structure. It impacts an estimated 10–15% of adults worldwide, with higher prevalence in women. A study reported 10.5% of adults had IBS, including 14% of women and 6.6% of men.
IBS Symptoms
- Abdominal cramping or discomfort.
- Periods of diarrhea, constipation, or alternating between both.
- Bloating or a feeling of a distended gut.
- Mucus in the stool.
- A sensation of incomplete bowel
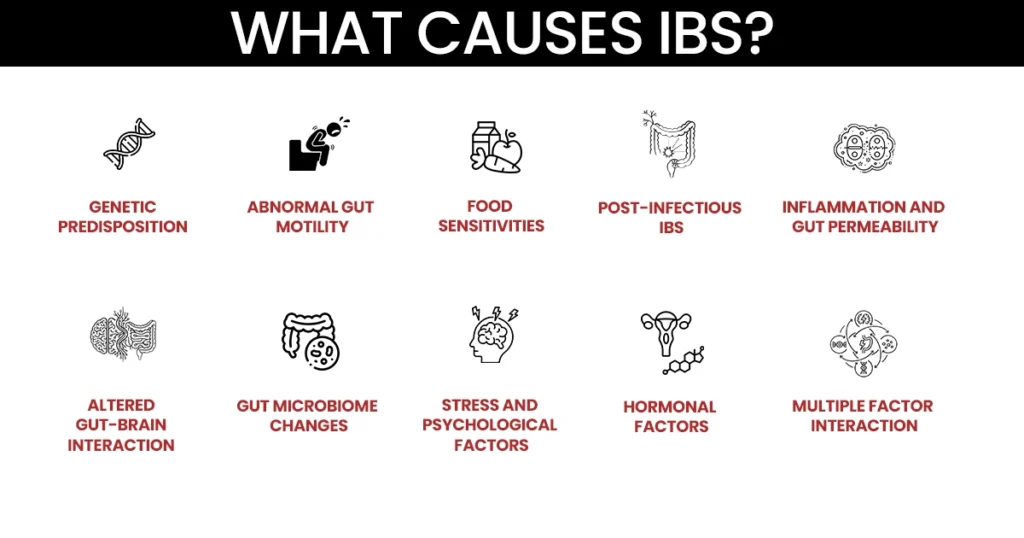
The exact cause of IBS remains unclear. It appears to result from a combination of factors that disrupt normal gut function and its communication with the brain. This complexity means IBS disease manifests differently in each person. Understanding potential causes helps guide effective management and symptom relief.
1. Genetic Predisposition
Genetics can increase susceptibility to IBS. If a close family member has IBS, you may be at higher risk, indicating inherited factors affect gut sensitivity and nervous system response. Genetics alone may not cause IBS, but combined with stress, diet, and environmental factors, they can trigger symptoms. Awareness of family history can aid in early recognition and proactive care.
2. Altered Gut-Brain Interaction
In many IBS cases, communication between the gut and brain is disrupted. Overly sensitive nerves in the intestines can make normal digestive processes, like gas or stool movement, painful. This explains why stress or anxiety can trigger IBS flare ups. Addressing gut-brain interactions is vital for symptom management.
3. Abnormal Gut Motility
Abnormal gut motility is common in IBS. Food moving too quickly can cause diarrhea, while slow movement can lead to constipation and painful bowel movements. Alternating diarrhea and constipation patterns (IBS-M) are linked to dysmotility. These changes affect digestion, nutrient absorption, and overall gut comfort.
4. Gut Microbiome Changes
The gut microbiome plays a critical role in digestion and immune function. Imbalances in gut bacteria or overgrowth in the small intestine can produce gas, bloating, and irregular bowel habits. SIBO can worsen symptoms like constipation after diarrhea or bloated gut pain. Restoring microbial balance can improve IBS symptoms significantly.
4. Food Sensitivities
Certain foods can irritate the gut and worsen symptoms. Common IBS trigger foods include high FODMAP items, fatty meals, caffeine, and artificial sweeteners. These can cause bloated gut pain, diarrhea, or constipation, triggering IBS flare ups. Identifying and avoiding trigger foods is essential for symptom control.
5. Stress and Psychological Factors
Stress, anxiety, and emotional strain can increase gut sensitivity and trigger painful bowel movements. If you frequently notice digestive discomfort during stressful periods, this may be related to stress-induced abdominal pain. Mental health care is an important aspect of IBS management.
6. Post-Infectious IBS
Some people develop IBS after severe gastrointestinal infections. These infections can alter gut sensitivity, motility, and microbiome composition. Symptoms like bloated gut pain, diarrhea, or constipation may persist even after recovery. Awareness of past infections can help explain symptom onset and guide treatment.
7. Hormonal Factors
IBS affects women nearly twice as often as men, indicating hormonal influences. Estrogen and progesterone fluctuations can impact gut motility and sensitivity, increasing IBS symptoms in females. Symptoms often worsen around menstrual cycles. Understanding these patterns helps with symptom management.
8. Inflammation and Gut Permeability
Subtle inflammation or increased gut permeability may contribute to IBS. These changes make the gut more reactive to food and digestive processes, causing bloated gut pain and altered bowel habits. Low-grade inflammation may also amplify responses to stress or IBS trigger foods. Addressing these factors can reduce flare ups.
9. Multiple Factor Interaction
IBS is often multifactorial, arising from interactions between genetics, gut-brain communication, microbiome imbalances, stress, and dietary triggers. This explains why IBS disease varies for each individual. Understanding these interactions is crucial for personalized treatment and long-term relief.
Warning Signs You Shouldn’t Ignore
While IBS is usually manageable, certain warning signs may indicate more serious conditions. Seek medical attention if you notice:
- Unexplained or severe weight loss.
- Persistent or worsening colon pain.
- Blood in stool or black, tarry stools.
- Nighttime symptoms that disrupt sleep.
- Fever, persistent vomiting, or dehydration.
- First onset of symptoms after age 50 or family history of colon cancer.
How Can IBS Be Treated?
IBS treatment focuses on reducing symptoms, improving quality of life, and managing flare ups. Effective management often combines lifestyle changes, diet, medication, and mental health support, tailored to each person’s IBS subtype.
- Diet & Lifestyle Adjustments: Adapting diet and eating habits can provide IBS relief. Avoiding trigger foods, eating smaller meals, and managing stress reduces bloated gut pain and painful bowel movements.
- Medications: Anti-diarrheal drugs, laxatives, antispasmodics, and low-dose antidepressants help manage IBS symptoms, reduce colon pain, and control diarrhea or constipation.
- Probiotics / Gut Microbiome Management: Balancing gut bacteria with probiotics can improve digestion and reduce IBS flare ups in those with SIBO or microbiome imbalances.
- Stress Management & Mental Health Therapies: CBT, mindfulness, and relaxation techniques help control stress, reducing IBS symptoms and preventing flare ups.
- Fiber & Nutritional Support: Adjusting fiber intake according to constipation or diarrhea patterns stabilizes bowel habits and supports digestive health.
- Personalized Treatment Based on IBS Subtype: IBS-C, IBS-D, and IBS-M require tailored approaches, as each subtype responds differently to treatments.
Find Relief from IBS at Texas Emergency Care Center
Dealing with digestive discomfort can make daily life difficult. Understanding what causes Irritable Bowel Syndrome is the first step toward managing symptoms. At Texas Emergency Care Center, our team provides expert care to identify triggers and guide you toward relief.
Whether you have frequent IBS flare ups or occasional digestive problems, professional evaluation can reduce discomfort and prevent complications. With support from Texas Emergency Care Center, you can improve gut health and find safe, effective relief from IBS symptoms.


