Blood clots can be silent threats with life-threatening consequences. Knowing the signs, causes, and risks associated with clots is essential for early detection and timely treatment. This blog will guide you through the different types of blood clots, how they affect various parts of the body, and when to seek emergency care for a blood clot.
Recognizing a blood clot emergency, such as sudden chest pain, swelling in the leg, or shortness of breath, can make all the difference. Understanding what to look for may help protect your health or even save someone else’s life.
What Is a Blood Clot?
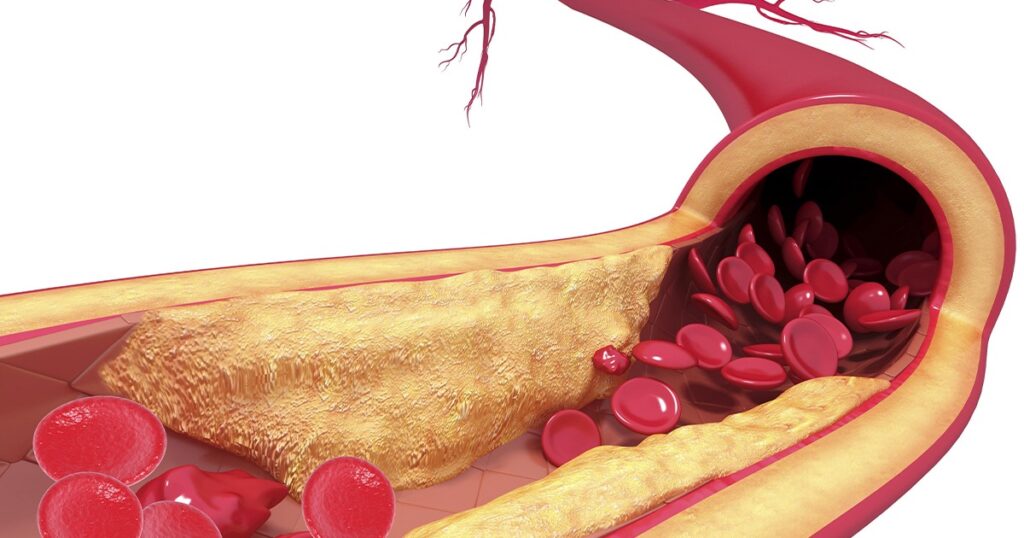
A blood clot is a semi-solid mass formed when blood thickens to stop bleeding. While this clotting process is vital after injury, blood clots that form inside the veins or arteries without trauma can disrupt circulation and lead to severe complications. These include deep vein thrombosis (DVT), pulmonary embolism (PE), heart attack, or stroke.
There are two major types of abnormal blood clots: arterial and venous. Arterial clots block oxygen-rich blood and can trigger strokes or heart attacks. Venous clots often form in the legs and can travel to the lungs, creating a pulmonary embolism.
Some clots dissolve naturally, but others can grow or travel through the bloodstream and cause life-threatening blockages. Recognizing symptoms early is essential to preventing serious outcomes.
Can You Have a Blood Clot Without Symptoms?
Yes, it is possible to have a blood clot with no obvious signs. Research shows that nearly half of the people with DVT have no noticeable symptoms. When symptoms do appear, they vary based on the clot’s location and severity. Prompt medical evaluation is crucial if you suspect a clot, even without clear indicators.
Blood Clot Symptoms by Location
Understanding where a clot forms can help you recognize the signs sooner and seek care faster.
Blood Clots in the Legs or Arms (Deep Vein Thrombosis)
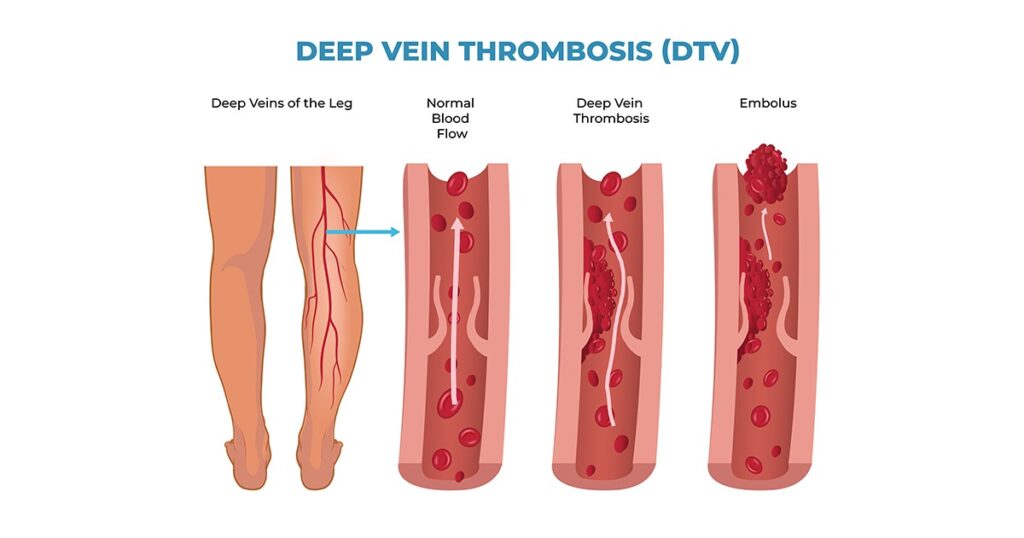
DVT is one of the most common forms of blood clots. It typically forms in the deep veins of the leg but can also affect the arms.
Symptoms may include:
- Swelling in the affected limb, usually one-sided
- Pain or cramping, often starting in the calf
- Skin that feels warm to the touch
- Tenderness in the leg or arm
- Red or purplish discoloration of the skin
Arterial clots in the limbs can cause reduced circulation, resulting in additional signs such as:
- Pale or bluish skin
- Numbness or tingling
- Coldness in the affected area
- Weakness or difficulty moving the limb
- Absent or weak pulse
These symptoms require immediate medical attention to prevent permanent damage or tissue death.
Blood Clots in the Heart (Coronary Artery Thrombosis)
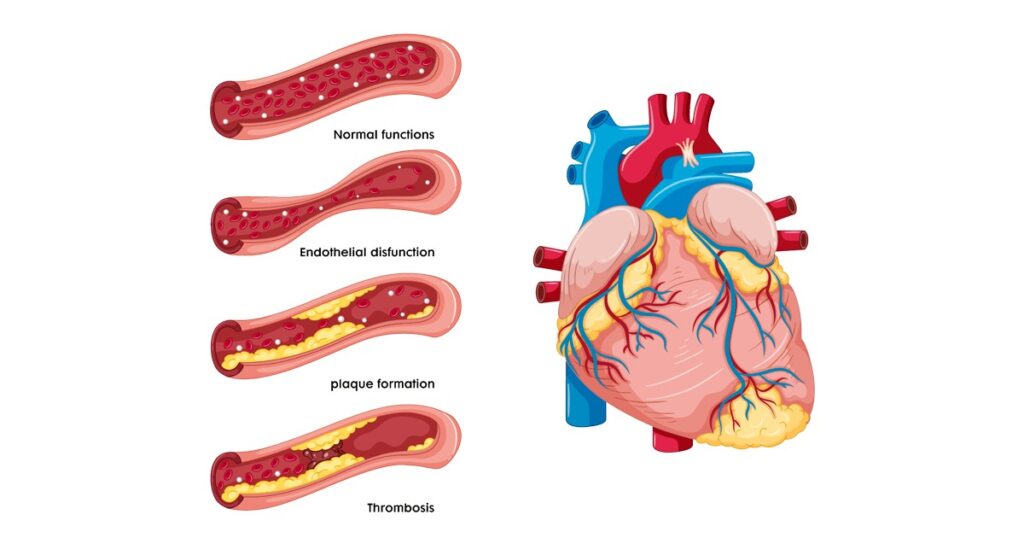
A clot in the heart’s arteries can reduce or stop blood flow to the heart muscle, resulting in a heart attack. This condition is known as coronary artery thrombosis.
Symptoms include:
- Intense or persistent chest pain or pressure
- Shortness of breath
- Pain that radiates to the neck, jaw, back, or arms
- Lightheadedness or fainting
- Excessive sweating
- Nausea or vomiting
These signs may develop suddenly or gradually and should never be ignored.
Blood Clots in the Abdomen
Clots in the abdomen can affect organs such as the intestines, spleen, or liver. These may form in veins or arteries and block the blood supply to internal tissues.

Possible symptoms include:
- Sudden or severe abdominal pain
- Pain that comes and goes unpredictably
- Abdominal swelling or bloating
- Nausea or vomiting
- Diarrhea or bloody stools
- Fluid buildup in the abdomen (ascites)
Because these symptoms can resemble other gastrointestinal disorders, diagnostic imaging is often necessary to confirm the presence of a clot.
Blood Clots in the Brain (Stroke)
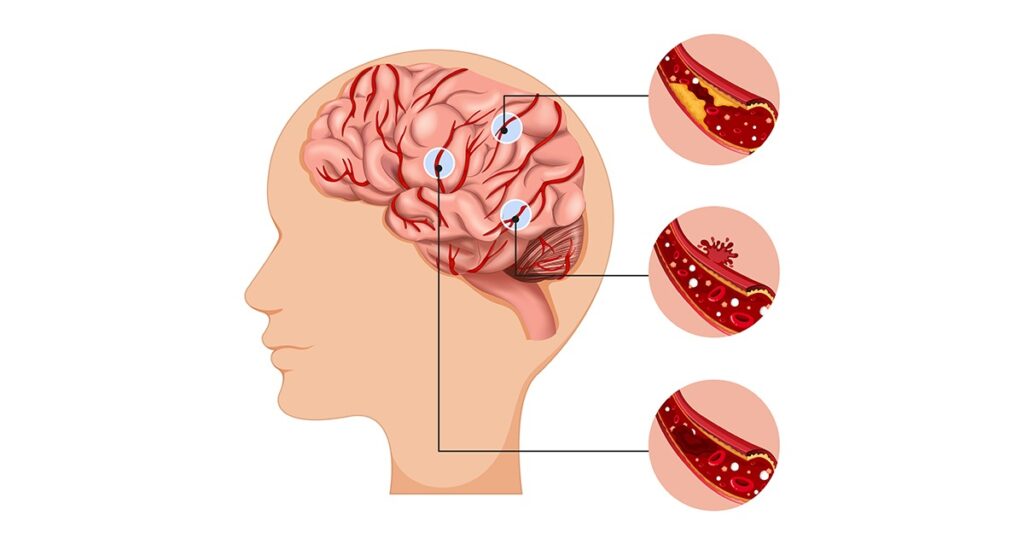
When a clot blocks blood flow to the brain, it can result in an ischemic stroke. This deprives brain tissue of oxygen and may cause irreversible damage within minutes.
Symptoms of a brain clot may include:
- Numbness or weakness in the face, arm, or leg, especially on one side of the body
- Sudden confusion or difficulty speaking
- Trouble understanding speech
- Vision changes in one or both eyes
- Dizziness or balance problems
- Sudden, severe headache with no known cause
- Loss of coordination or consciousness
- Nausea or vomiting
Even brief symptoms may signal a transient ischemic attack, often called a mini-stroke, which requires immediate evaluation to prevent a major stroke.
Blood Clots in the Lungs (Pulmonary Embolism)
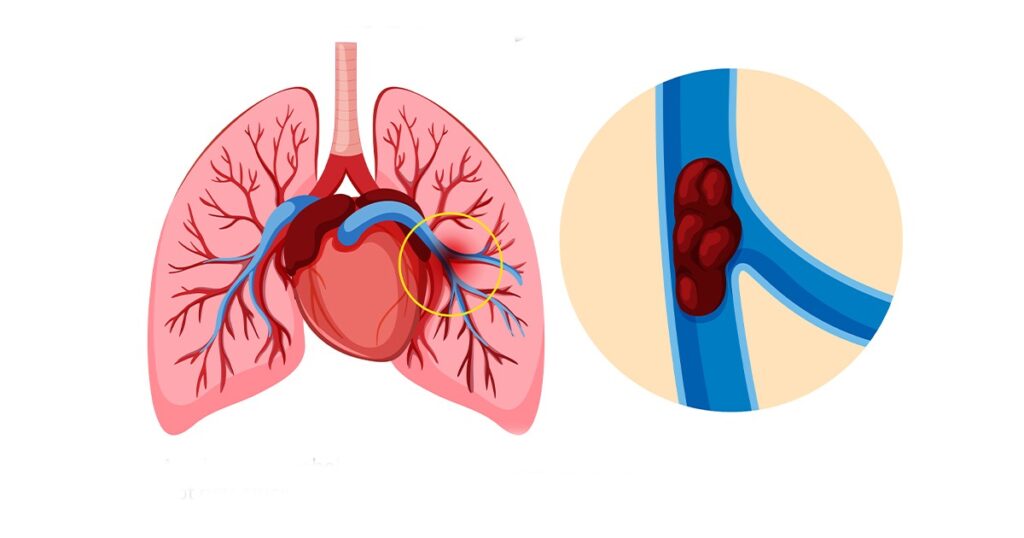
A pulmonary embolism occurs when a clot, often from the leg, travels to the lungs and blocks an artery. This is a medical emergency that can lead to heart failure or death if untreated.
Symptoms may include:
- Sudden shortness of breath unrelated to physical activity
- Sharp chest pain that worsens when breathing deeply
- Rapid or irregular heartbeat
- Coughing, sometimes with blood
- Lightheadedness, fainting, or feeling anxious
Pulmonary embolisms can be fatal, and any suspected symptoms should be treated as an emergency.
Blood Clots in Children
Although uncommon, children can develop blood clots, especially when hospitalized or undergoing medical treatment. Factors that increase the risk in children include:
- Reduced mobility due to illness or injury
- Use of central venous catheters
- Genetic clotting disorders
- Abnormal blood vessel formation
- Certain medications or treatments for chronic conditions
Because symptoms may be harder to detect in children, any unexplained swelling, pain, or change in behavior should be evaluated promptly by a healthcare provider.
Treatment Options for Blood Clots
Treatment depends on the clot’s size, location, and risk level. Common approaches include:
- Anticoagulants (blood thinners) to prevent clot growth and formation
- Thrombolytics to dissolve large or life-threatening clots quickly
- Surgical removal of the clot in extreme cases
- Insertion of a filter in the vena cava to block clots from reaching the lungs
- Compression stockings to reduce swelling and prevent clot recurrence
Some people may require long-term anticoagulant therapy to manage chronic risk factors.
How to Reduce Your Risk of Blood Clots
There are several lifestyle changes and medical steps that can lower your risk:
- Stay physically active, especially during travel or recovery from surgery
- Maintain a healthy weight and avoid prolonged periods of inactivity
- Drink plenty of water to prevent blood thickening
- Quit smoking, as it damages blood vessels and increases clotting risk
- Follow your doctor’s advice if you take hormonal medications or have a clotting disorder
- Monitor and manage chronic health conditions such as high blood pressure or diabetes
If you are scheduled for surgery or have other risk factors, talk to your doctor about preventive strategies before complications arise.
Visit Texas ER for Expert Emergency Care
If you experience symptoms such as unexplained leg swelling, chest pain, difficulty speaking, or sudden shortness of breath, do not wait. Early diagnosis and treatment are critical to preventing serious complications.
Texas Emergency Care Center provides 24/7 emergency services with experienced, board-certified physicians ready to diagnose and treat blood clots and related conditions. With advanced imaging technology, fast lab results, and no wait times, you can get the care you need when every minute counts.


